What is FastGlioma? A Game-Changing AI Model
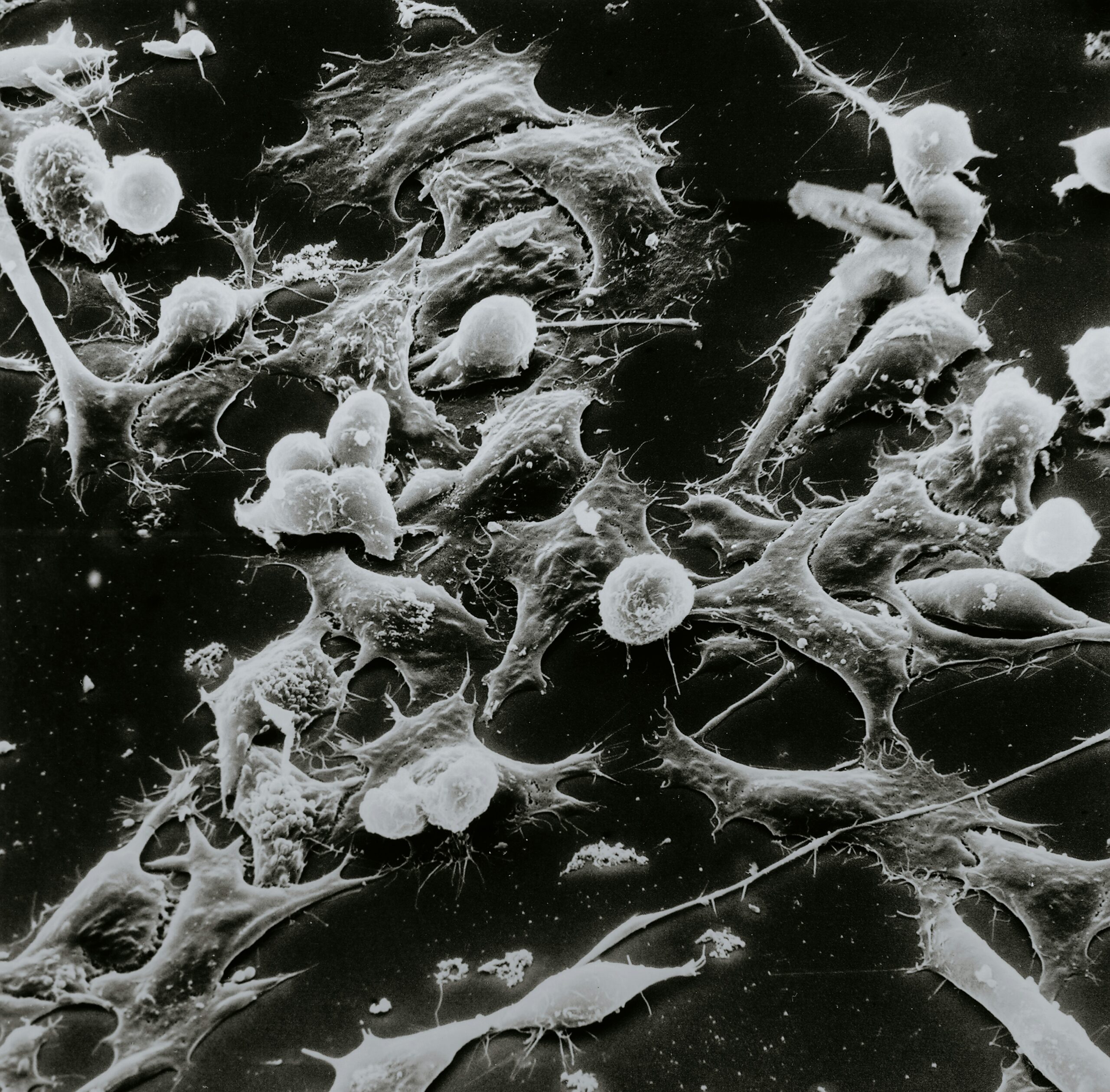
FastGlioma is an innovative artificial intelligence tool developed by researchers at the University of Michigan, designed to revolutionize the detection of cancerous brain tumors in surgical settings. Utilizing advanced machine learning algorithms, FastGlioma scans surgical areas and analyzes complex data in a remarkably short timeframe of just 10 seconds. This rapid assessment allows neurosurgeons to make swift and informed decisions regarding the presence of tumors, significantly enhancing the surgical process.
In contrast to traditional histopathology methods, which often require hours or even days for analysis, FastGlioma offers a transformative approach that emphasizes speed and accuracy. The AI model is capable of differentiating between tumor tissue and healthy tissue with a high degree of precision. This capability is particularly critical during surgery, as it reduces the risk of leaving malignant tissue behind, ultimately leading to more favorable patient outcomes.
The implementation of FastGlioma in operating rooms not only saves valuable time but also increases the likelihood of complete tumor removal. With the capacity to deliver instantaneous results, surgeons can adjust their strategies on the spot, optimizing the effectiveness of the surgery. Furthermore, the AI model has undergone extensive testing, demonstrating superior performance when benchmarked against conventional processes. Such advancements in medical technology underscore the potential of AI to enhance surgical practices in oncology.
As FastGlioma continues to gain recognition, its integration into surgical workflows represents a pivotal shift towards the future of cancer treatment. By bridging the gap between rapid diagnostics and surgical execution, this AI tool exemplifies how technology can improve healthcare delivery and patient care, showcasing a significant leap forward in the fight against cancer.
The Impact of FastGlioma on Neurosurgery
FastGlioma represents a significant advancement in the realm of neurosurgery, particularly in the management of diffuse gliomas, which are notoriously challenging due to their infiltrative nature. This innovative tool drastically reduces the time required for tumor detection during surgery, facilitating crucial decision-making processes within the operating room. By providing real-time analysis, FastGlioma enables neurosurgeons to conduct more comprehensive tumor resections. This capability is paramount, as incomplete removal of gliomas can lead to higher recurrence rates and poorer patient outcomes.
The integration of FastGlioma into surgical practice not only enhances the precision of brain tumor excisions but also empowers medical professionals to make informed judgments on the extent of resection necessary. This leads to improved patient survival rates as oncology teams can more confidently pursue aggressive surgeries with an understanding of the tumor’s margins. Moreover, minimizing the risk of leaving residual tumor cells can significantly mitigate the likelihood of tumor recurrence, a critical consideration in the management of gliomas.
Looking beyond gliomas, the technology underlying FastGlioma has potential applicability across various cancer types. The rapid detection capabilities may be adapted for use in surgeries targeting other oncological challenges, thereby transforming surgical standards and improving outcomes in a broader context. As oncological surgery continues to evolve with technological advances, tools like FastGlioma will likely reshape the landscape of cancer treatment. It sets a new benchmark in surgical oncology, emphasizing the importance of prompt and accurate tumor identification to enhance the efficacy of interventions and elevate overall patient care.
Challenges and Future Directions
The integration of artificial intelligence (AI) into surgical practice presents both significant challenges and promising future directions. One of the foremost obstacles is the need for adequate training for surgeons who will be utilizing these advanced tools during operations. It is essential that medical professionals not only become familiar with the technology itself but also understand how to interpret AI-generated data effectively. This positions AI as a collaborative aid rather than a replacement, requiring a paradigm shift in both education and surgical methodologies.
Additionally, the quality of data used to train AI systems plays a pivotal role in their accuracy. AI’s ability to detect cancerous brain tumors relies on access to high-quality, diverse datasets that accurately reflect various cases. If the training data is biased or limited, the efficacy of AI in real-world applications may be compromised. Ongoing collaboration between research institutions, data scientists, and healthcare professionals is crucial for creating robust datasets that can enhance the performance of tools like FastGlioma.
Moreover, looking ahead, there exists a considerable potential for expanding the applications of FastGlioma beyond brain tumors. Other oncology disciplines may greatly benefit from similar AI interventions, paving the way for quicker diagnostics and improved surgical outcomes across diverse cancer types. This advancement could enhance patient management strategies, streamline surgical processes, and ultimately lead to more effective treatment regimens. Future research should focus on how AI can be tailored to address specific characteristics of various cancers, allowing for more personalized and precise patient care.
In conclusion, while the path to integrating AI in surgical settings is fraught with challenges, strategic training, quality data, and a commitment to expanding applications hold the promise of revolutionary changes in cancer treatment and surgical practices.
Ethical Considerations in AI Healthcare Implementation
The integration of artificial intelligence in healthcare, particularly in critical areas such as surgery, brings forth significant ethical considerations that must be addressed. One of the paramount concerns is data privacy, as AI systems often rely on vast amounts of patient data for training and operation. Ensuring that patient information is handled with the utmost confidentiality is critical. This necessitates adherence to regulations such as the Health Insurance Portability and Accountability Act (HIPAA) to safeguard sensitive health information.
Moreover, transparency plays a crucial role in establishing a foundation of trust between healthcare providers and patients. Patients must be made aware of how AI systems function, including the data they utilize and the decision-making processes involved in diagnosing conditions like cancerous brain tumors. Clear communication about the capabilities and limitations of AI technology is essential to foster an understanding of its role in improving surgical outcomes. Ensuring that patients grasp the AI’s involvement without overshadowing the clinical expertise of surgeons is vital to maintaining their confidence in medical decisions.
Additionally, rigorous testing and professional validation of AI models must be prioritized. The ethical deployment of AI in medical settings mandates that these systems undergo extensive evaluation before being introduced to clinical practice. This includes validating accuracy, reliability, and effectiveness in real-world scenarios, particularly in high-stakes environments such as surgery. Professional endorsement from medical communities, alongside independent reviews, can further lend credibility to AI technologies, thereby reinforcing patient trust.
In navigating these ethical considerations, it is also vital for healthcare providers to engage patients and their families in conversations about AI utilization. Establishing a collaborative dialogue can facilitate understanding and alleviate any concerns related to the technology’s role during procedures. By prioritizing transparency, rigorous evaluations, and ethical data handling, the integration of AI in healthcare can achieve a balance that respects patient rights and enhances overall care.
Building Patient Confidence in AI
As artificial intelligence (AI) continues to revolutionize the medical field, particularly in the rapid detection of cancerous brain tumors during surgery, it is imperative to focus on building patient confidence in these technologies. One essential strategy is fostering transparent communication concerning AI’s role in treatments. Patients are often apprehensive about the implications of AI in their healthcare, and addressing these concerns directly can alleviate anxiety. Clear explanations of how AI systems function, the precision they offer, and their ability to enhance traditional methods of diagnosis can reassure patients. Detailed discussions regarding data sources, algorithms, and the mechanics of AI applications help demystify the technology and make it more approachable.
Another significant aspect involves actively engaging with patient concerns. Healthcare providers should encourage open dialogue that invites questions about the AI processes and its decision-making capabilities. When patients feel heard and acknowledged, they are more likely to trust the evaluation and recommendations provided by both AI and medical teams. This engagement can be supplemented through various forums, including workshops, informational sessions, and direct consultations, emphasizing the collaborative aspect of human-AI partnerships in healthcare.
Additionally, the availability of educational resources plays a critical role in patient empowerment. Providing accessible materials, such as pamphlets, videos, or online courses related to AI in healthcare, can significantly enhance understanding of its benefits and limitations. Offering content that demystifies AI tools utilized in detecting brain tumors or other medical conditions promotes a more informed decision-making process among patients. When individuals comprehend the potential advantages of AI, alongside a realistic acknowledgment of its limitations, they can interact more confidently with their healthcare providers, ultimately leading to better healthcare experiences overall.
Recommended Reading for AI in Medicine Enthusiasts
For those intrigued by the profound impact of artificial intelligence in healthcare, exploring comprehensive literature on the subject can be incredibly enlightening. One notable recommendation is the book titled Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again by Eric Topol. This transformative work delves into the intersection of advanced technology and the essential human element in medical practice, providing a nuanced understanding of how AI can enhance the healthcare experience.
In Deep Medicine, Topol discusses the evolution of artificial intelligence, highlighting its capabilities and potential applications within the medical field. He emphasizes the need for a balance between technological advancements and the compassionate aspect of patient care. This balance is crucial, particularly in fields such as surgical practices, where rapid diagnostics and personalized treatment plans can significantly improve patient outcomes. The book offers valuable insights into the ethical considerations surrounding AI, addressing concerns about data privacy, bias in algorithms, and the importance of maintaining human oversight.
Moreover, readers will find Topol’s perspective on the future of healthcare particularly thought-provoking. He argues that as AI systems become increasingly integrated into medical practices, they can augment physicians’ abilities, facilitating better decision-making and more accurate diagnoses. This is especially relevant in cases involving complex conditions such as cancerous brain tumors, where time is of the essence during surgeries. By understanding how AI can support medical professionals, readers will gain a broader appreciation for its role in revolutionizing the healthcare landscape.
For those interested in further exploring this engaging topic, Deep Medicine by Eric Topol is an essential read that offers a deep dive into the potential of AI in medicine. This book serves as a crucial guide for anyone looking to comprehend the transformative capabilities of AI technology in healthcare.
Conclusion: The Future of AI in Medicine
The introduction of FastGlioma, an AI tool that can accurately detect cancerous brain tumors in just 10 seconds during surgery, marks a significant leap forward in the realm of medical technology and treatment. This breakthrough is not only vital for the immediate surgical processes but also has far-reaching implications for patient outcomes. The ability to swiftly identify malignant tumors allows surgeons to make more informed decisions in real-time, potentially reducing the need for follow-up surgeries and improving the overall prognosis for patients diagnosed with brain cancer.
Moreover, FastGlioma serves as a testament to the growing role of artificial intelligence in enhancing medical diagnostics and treatments. As AI technology continues to evolve, we can anticipate further innovations that may redefine the landscape of healthcare, streamlining procedures, enhancing accuracy, and ultimately saving lives. The integration of AI in surgical environments could pave the way for safer, more efficient operations, highlighting AI’s relevance in addressing complex medical challenges.
It is important for healthcare professionals, researchers, and patients alike to consider the implications of such technological advancements. The role of AI in surgeries raises numerous questions and discussions surrounding ethics, data privacy, and the potential for replacing human expertise. As vital stakeholders in the healthcare ecosystem, consider how AI might affect your practice or experience and what it means for the future of patient care.
We invite readers to share their thoughts and opinions regarding AI’s role in surgical procedures and cancer detection in the comments section. Your insights could greatly enrich the conversation surrounding this transformative technology. Looking ahead, it is imperative that we continue to explore the potential of AI within the healthcare field, unveiling its capabilities and harnessing its benefits to improve lives worldwide.
External Resources on AI in Healthcare
For readers who wish to explore the groundbreaking advancements in artificial intelligence (AI) within the healthcare sector, several resources offer in-depth insights and comprehensive analyses. One such valuable source is the National Institutes of Health (NIH), which regularly publishes research findings and explores the integration of AI technologies in various medical practices. Their reports highlight how AI algorithms are enhancing diagnostic accuracy, streamlining surgical procedures, and improving patient outcomes. By visiting their official website, readers can access a wealth of information detailing the latest studies focused on AI in oncology, specifically in the realm of brain tumor detection.
Another excellent resource is the journal “Nature Medicine,” which delves into cutting-edge medical research and the application of AI across different specialties. This peer-reviewed journal features articles that discuss the development of AI tools capable of analyzing medical imaging data rapidly and efficiently. Such studies underscore the ongoing innovation in the medical field as AI becomes instrumental in the early detection of cancerous cells and tumors during surgeries.
Moreover, tech-oriented platforms like MIT Technology Review provide periodic articles and analyses on how AI is influencing healthcare, including interviews with leading experts working in the field. These articles can offer unique perspectives on the challenges and opportunities that arise from implementing AI technologies in medical settings.
For those interested in the practical applications of AI in the operating room, industry publications often share case studies demonstrating successful outcomes. Exploring these external links will deepen your understanding of AI’s transformative impact on healthcare and its promise for the future of patient care.
Discussion and Community Engagement
The introduction of AI technologies in healthcare has paved the way for remarkable transformations. The recent advancements exhibited by FastGlioma, particularly in the rapid detection of cancerous brain tumors during surgery, present an opportunity for us to engage in a meaningful discussion. As this groundbreaking artificial intelligence application demonstrates its potential to enhance surgical outcomes and precision, it raises pertinent questions concerning the integration of such innovations into standard medical practices.
The implications of AI in cancer treatment go beyond merely improving detection times. They extend into the realms of accuracy, safety, and patient experience. By significantly reducing the time it takes to identify malignant tissues, FastGlioma not only increases the likelihood of successful surgical interventions but also enhances the confidence of both patients and healthcare providers in making critical decisions. This prompts a dialogue about the ethical considerations involved in AI-assisted surgeries and the responsibilities of medical professionals in harnessing AI tools.
We invite our readers to share their thoughts and experiences regarding AI in healthcare. Perhaps you have witnessed or participated in a clinical setting where artificial intelligence played a crucial role. How do you perceive the changes it brings to patient care? Does the speed and accuracy of AI systems allay your concerns, or do you have reservations about their implementations? Your insights contribute to a richer understanding of the societal impact of these technologies.
Engagement in this conversation is vital. By sharing your perspectives in the comments section, you help cultivate a community that values dialogue surrounding innovative solutions in medical practices like FastGlioma. Through collaboration and shared experiences, we can explore the future of healthcare and the role of AI in enhancing our collective well-being.
Future Innovations in AI and Healthcare
The vast potential of artificial intelligence (AI) technology is already making waves in healthcare, particularly in the diagnosis and treatment of conditions such as cancer. As AI continues to evolve, it is anticipated that future innovations will significantly enhance patient care, surgical techniques, and diagnostic methods. Key areas of advancement are likely to revolve around machine learning and data analytics, which could lead to more precise predictions about disease progression.
In the realm of surgical techniques, AI could pave the way for robotic-assisted surgeries that require minimal human intervention. With advancements in real-time imaging and AI-integrated systems, surgeons may soon have access to augmented reality overlays, providing an enhanced view of critical structures and enabling more precise interventions. Such innovations could contribute to reduced recovery times and improved outcomes for patients.
Furthermore, the integration of AI with wearable health technology holds great promise for continuous monitoring of patient health. Innovations in AI could enable early detection of anomalies, facilitating timely intervention and effective management of chronic diseases. Predictive analytics may also become a cornerstone of personalized medicine, where treatment plans are customized based on an individual’s genetic makeup and lifestyle. This focused approach could revolutionize the way treatments are administered, making them more effective and reducing adverse side effects.
Moreover, as AI technology advances, the potential to streamline administrative processes will not go unnoticed. Automating routine tasks, such as patient scheduling and billing, could free up healthcare professionals to concentrate on patient care, thereby enhancing overall efficiency and satisfaction.
All these prospects suggest that the future of AI in healthcare may bring about transformative changes that improve patient outcomes and optimize healthcare delivery. The continuous interplay between AI innovations and healthcare practices will be crucial in building a more effective system for managing crises like cancer diagnosis and treatment.