Introduction to Antifungal Resistance
Antifungal resistance refers to the ability of fungal pathogens to withstand the effects of antifungal medications, rendering these treatments ineffective. This phenomenon has emerged as a significant concern within the realm of global health, particularly in light of the increasing incidence of fungal infections across various populations. In recent years, the prevalence of these infections has been on the rise, leading to heightened alarm among healthcare professionals and researchers alike.
Fungal infections pose a serious threat, especially to immunocompromised individuals, such as those undergoing chemotherapy, organ transplant recipients, and patients with HIV/AIDS. The World Health Organization (WHO) has recognized the growing burden of fungal diseases, indicating that invasive fungal infections account for millions of deaths annually. Furthermore, it is estimated that around 1.5 million people succumb to such infections each year, showcasing the significant impact these diseases have on public health.
Compounding the challenge of managing fungal infections is the alarming rate at which antifungal resistance is developing. Many common antifungal agents, including azoles and echinocandins, are becoming less effective due to the emergence of resistant strains of fungi. According to a recent report by the Global Action Fund for Fungal Infections, over 90% of some fungal species tested exhibit varying degrees of resistance to standard treatments. This situation not only complicates clinical management but also increases healthcare costs and patient morbidity.
The rise of antifungal resistance necessitates a multifaceted approach to combat this emerging threat. Improved diagnostic techniques, infection prevention measures, and enhanced stewardship of existing antifungal agents are critical components of the response. As researchers and public health officials confront the challenge of antifungal resistance, addressing this issue becomes imperative to protect vulnerable populations and reduce the global burden of fungal diseases.
The Threat of Antifungal Resistance
Antifungal resistance has emerged as a significant threat to public health, with serious implications for individuals and healthcare systems alike. The rise of resistant fungal strains can be largely attributed to the overuse and misuse of antifungal medications, which has created a selective pressure that allows these organisms to thrive. Frequently, antifungals are prescribed for conditions where they are not warranted, leading to the survival of strains that can no longer be effectively treated by standard medications. This mismanagement not only increases healthcare costs but also compromises the effectiveness of current treatment protocols, making it increasingly difficult to manage fungal infections.
In addition to the inappropriate use of antifungal agents, inadequate public health measures have played a crucial role in the proliferation of antifungal resistance. Surveillance systems that monitor fungal infections and their resistance patterns are often underfunded or non-existent in many regions. This lack of proactive measures hampers our understanding of the epidemiology of resistant strains, ultimately hindering efforts to contain outbreaks. As resistance spreads, previously treatable infections become difficult, if not impossible, to treat, posing heightened risks to at-risk populations, including immunocompromised individuals and those undergoing extensive medical procedures.
Real-world examples of outbreaks of resistant fungal infections underscore the urgency of addressing antifungal resistance. Notable incidents, such as the emergence of Candida auris, have highlighted the dangerous ramifications of this growing issue. Initially identified in 2009, Candida auris has since been linked to widespread outbreaks across various healthcare facilities worldwide. Its resistance to multiple antifungal classes has resulted in treatment failures and alarmingly high mortality rates. As more cases of resistant fungal species come to light, it becomes increasingly essential for both healthcare professionals and policymakers to take immediate action to combat antifungal resistance and safeguard public health.
Recent Research Findings
Recent studies have highlighted the alarming rise of antifungal resistance in various fungal pathogens, prompting significant concern among researchers and healthcare professionals alike. A pivotal study published in the Journal of Antimicrobial Chemotherapy examined the adaptive mechanisms of Candida auris, a notorious multidrug-resistant fungus. The researchers employed whole-genome sequencing to identify mutations linked to resistance, which revealed that these fungi can develop resistance rapidly, sometimes within weeks of exposure to antifungal agents.
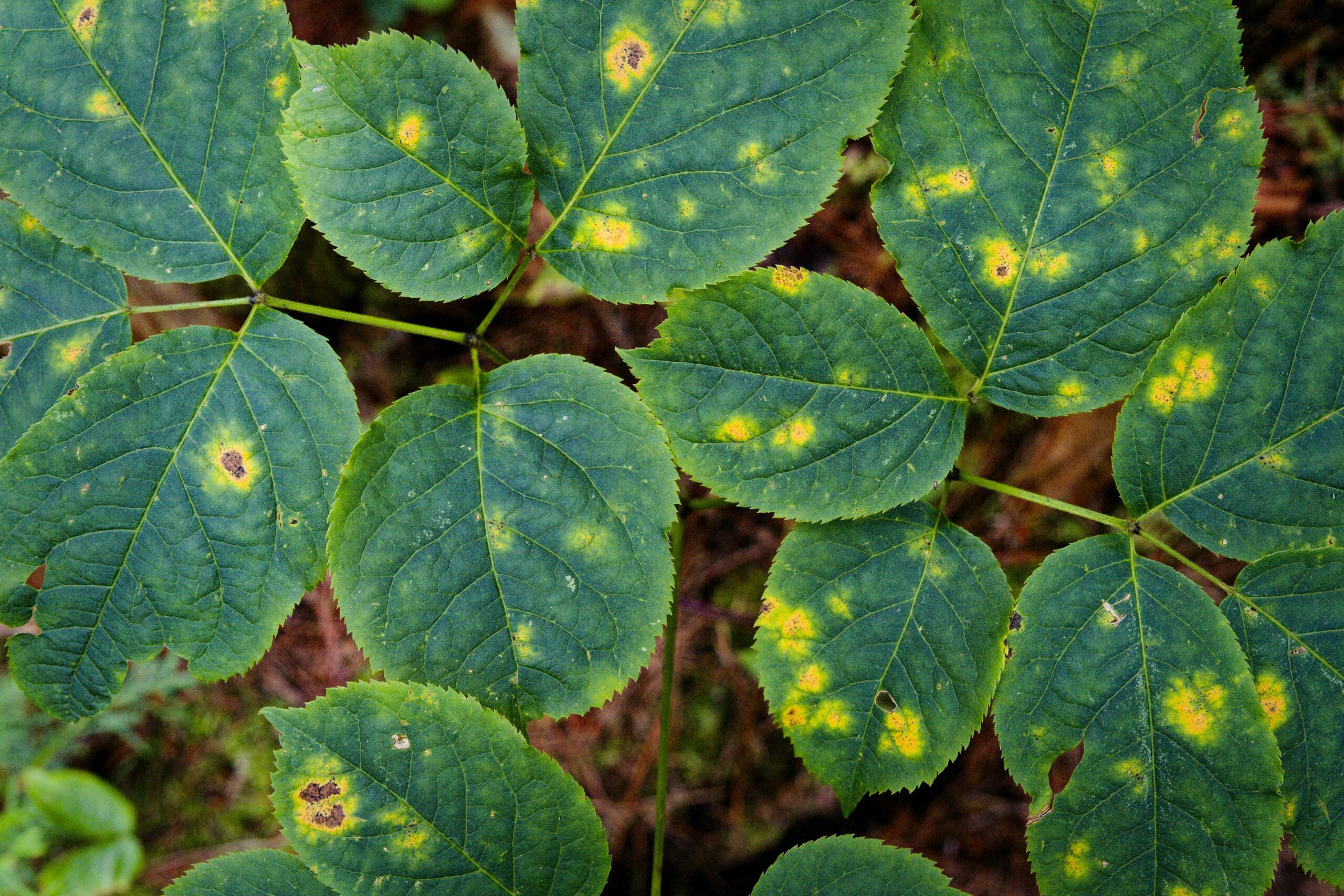
Another critical study conducted by the Centers for Disease Control and Prevention (CDC) focused on the emergence of resistant Aspergillus fumigatus strains. Through longitudinal sampling and environmental assessments, the team discovered a marked increase in isolates with mutations in the azole resistance gene, which are often found in agricultural settings due to the extensive use of antifungal agents. These findings underscore the necessity of understanding the evolutionary pressures exerted by both clinical and agricultural practices on fungal populations.
Furthermore, researchers at the University of Maryland investigated the role of biofilms in antifungal resistance. Their study utilized advanced imaging techniques and in vitro models to demonstrate that Candida species in biofilm formations exhibit a significantly higher resistance to commonly used antifungal drugs. This discovery suggests that targeting biofilm-related mechanisms may be a crucial avenue for future therapeutic strategies.
The ongoing research in this field also shines a spotlight on innovative approaches to counteract antifungal resistance. A collaborative study published in Nature Microbiology introduced a novel combination therapy utilizing established antifungals with natural compounds derived from plant extracts. This synergy was shown to enhance antifungal efficacy against resistant strains, highlighting a promising direction for future investigations.
Collectively, these groundbreaking findings emphasize the need for urgent action in addressing antifungal resistance. The adaptability of fungi poses a substantial threat to public health, necessitating coordinated global efforts for surveillance, research, and improved therapeutic strategies.
Voices of Experts: Scientists Sound the Alarm
Antifungal resistance represents an escalating threat to public health, as recognized by leading scientists in the fields of mycology and infectious diseases. Dr. Jennifer Smith, an esteemed mycologist, emphasizes the urgency of this issue by stating, “Antifungal resistance has reached a point where common fungal infections are becoming increasingly challenging to treat. We are witnessing a troubling rise in resistant strains, and without immediate action, we risk losing effective treatment options.” This sentiment is echoed across the scientific community, underscoring the need for a unified response to combat this emerging crisis.
Furthermore, Dr. Michael Patel, an infectious disease specialist, highlights the multifaceted nature of this problem: “The overuse and misuse of antifungal medications in clinical settings have led to a breeding ground for resistant organisms. To protect the efficacy of existing therapies, it is paramount that healthcare providers adhere to strict prescribing guidelines and consider alternative treatment strategies when appropriate.” These statements reflect a growing consensus that a reevaluation of current practices is essential to mitigating the impact of antifungal resistance.
Leading scientists are not only calling for better stewardship of antifungal agents but also advocating for innovative research into new therapies. Dr. Linda Zhou, an expert in pharmaceutical research, notes, “Investing in the discovery of novel antifungal compounds is crucial. Leveraging new technologies and approaches could pave the way for combination therapies that enhance efficacy or target resistant strains more effectively.” This proactive approach could potentially reshape the landscape of antifungal treatment, providing hope in the face of a daunting challenge.
As the scientific community rallies around this critical issue, it becomes increasingly clear that collaboration is key. By fostering partnerships between academia, healthcare, and pharmaceutical industries, we can ensure that both current and future antifungal therapies remain effective against the growing threat of resistance.
The Human Cost of Antifungal Resistance
The impact of antifungal resistance on individuals and families is profound, often extending beyond the confines of clinical statistics into the very fabric of daily life. Many patients suffering from resistant fungal infections endure not only the physical toll of their illness but also significant emotional and financial distress. Take, for instance, the story of Maria, a mother in her forties who experienced a severe Candida infection that was resistant to standard treatments. After multiple hospitalizations, Maria faced a frustrating journey that left her feeling isolated and helpless. The persistent pain and recurrent symptoms made it difficult for her to engage with her children, leading to an emotional burden that weighed heavily on the entire family.
This personal experience is echoed by countless others who find themselves caught in the relentless grip of antifungal-resistant infections. For many, the journey includes numerous treatments and therapies that prove ineffective, resulting in prolonged suffering and hardship. Patients often express feelings of despair and uncertainty, as they grapple with the inability to return to normalcy in their lives—emotionally, physically, and socially. This suffering is not only personal; it reverberates through families, creating an atmosphere of worry and distress as loved ones attempt to provide support.
Financially, the burden can be staggering. The costs associated with advanced medical treatment, ongoing hospital stays, and medications can overwhelm families, leading to financial instability or even bankruptcy. In addition to direct medical expenses, patients may also lose income due to time away from work or the inability to maintain regular employment. Each story of a person impacted by antifungal resistance serves as a reminder of the urgent need to address this crisis, not only for the sake of public health but for the well-being of individuals who are facing the harsh realities of these infections. The human cost of antifungal resistance is evident and cannot be overlooked.
Global Strategies to Combat Antifungal Resistance
Antifungal resistance poses significant challenges to global health, necessitating coordinated efforts from various stakeholders. The World Health Organization (WHO) has recognized the need for a comprehensive framework to address this issue. Key initiatives include the establishment of the Global Action Plan on Antimicrobial Resistance, which emphasizes enhancing surveillance of antifungal resistance patterns and the importance of stewardship programs. These programs aim to promote the responsible use of antifungals in healthcare settings, thereby reducing the selection pressure that contributes to resistance development.
In addition to WHO’s global initiatives, local health agencies are mobilizing resources to combat antifungal resistance within their jurisdictions. Interventions often focus on improving laboratory capacity for accurate diagnosis, which is essential for targeting appropriate therapies. By ensuring timely and precise identification of fungal pathogens, healthcare providers can make informed decisions regarding antifungal treatments, minimizing unnecessary usage that can lead to resistance emergence.
Furthermore, educational campaigns are being carried out to raise awareness among healthcare professionals and the public about the prudent use of antifungals. This knowledge dissemination aims to foster a culture of safety, where both prescribers and patients understand the potential consequences of misuse. In this context, the involvement of various sectors, including veterinary and agricultural fields, is crucial as antifungal agents are frequently used in these areas, contributing to the overall burden of resistance.
Another notable strategy is the promotion of research and development (R&D) for novel antifungal agents. Collaboration between governments, academic institutions, and pharmaceutical companies is encouraged to facilitate the discovery of new compounds that can effectively combat resistant fungal strains. Ultimately, a multifaceted approach combining surveillance, education, stewardship, and innovation will be essential for controlling antifungal resistance globally.
Preventive Measures for Patients and Healthcare Providers
Antifungal resistance poses a serious threat to public health, necessitating diligent preventive measures from both patients and healthcare providers. Effective strategies begin with proper prescribing practices. Healthcare providers should adhere to evidence-based guidelines that inform the choice of antifungal medication, avoiding unnecessary prescriptions and considering narrower spectrum options when appropriate. This targeted approach can significantly reduce the risk of developing resistant strains of fungi.
In addition to careful prescribing, patient education is vital in combating antifungal resistance. Healthcare professionals should engage in thorough discussions with patients regarding the importance of completing full courses of antifungal treatments as prescribed. Educating patients about the risks associated with the misuse or overuse of these medications can lead to more informed decisions and better adherence to treatment regimens. Involving patients in their treatment plan fosters a sense of responsibility toward not only their health but also the broader community.
Maintaining hygiene standards within healthcare settings is another critical preventive measure. Regular cleaning and sanitization of medical facilities can minimize the potential for fungal infections. Healthcare providers should emphasize the need for proper hand hygiene and infection control protocols, especially in environments where patients are at higher risk. Establishing a culture of cleanliness and vigilance can help reduce the incidence of infections that may require antifungal treatment.
Lastly, fostering interdisciplinary collaboration among healthcare professionals enhances the effectiveness of these preventive strategies. A collective commitment among doctors, nurses, pharmacists, and infection control specialists is essential for promoting best practices and minimizing the emergence of antifungal resistance. By working together, the healthcare community can take significant strides toward safeguarding patients’ health and mitigating the risks associated with fungal diseases.
The Role of Public Awareness and Education
Public awareness and education play a crucial role in addressing the growing challenge of antifungal resistance in fungal diseases. As resistant strains of fungi continue to emerge, it becomes increasingly vital for communities to be informed about the risks associated with fungal infections and the importance of effective treatments. Education initiatives can empower individuals to recognize the symptoms of fungal infections early, which can lead to timely medical intervention and, ultimately, improved health outcomes.
Awareness campaigns should focus on the importance of adherence to prescribed treatment regimens. Many individuals may not follow through with their antifungal treatments due to a lack of understanding about the necessity of completing the course, or misunderstanding the severity of their condition. When patients do not adhere to these treatment plans, they not only risk their own health but also contribute to the potential development of antifungal-resistant strains. Educational measures, including informational brochures, workshops, and digital resources, can significantly enhance comprehension regarding treatment importance, thereby promoting better health practices among the public.
Furthermore, outreach programs can facilitate direct engagement with at-risk populations, particularly those in areas with limited access to healthcare resources. Collaboration with healthcare professionals, community leaders, and educators can pave the way for workshops and seminars that encourage discussion about fungal infections and resistance. Media channels, including social media, can also be leveraged to disseminate information widely and rapidly, ensuring maximum reach. By fostering a well-informed public, the chances of impeding antifungal resistance can be substantially increased, thereby contributing to overall public health stability.
In conclusion, enhancing public awareness and education is essential in the fight against antifungal resistance. Through proactive engagement and informed communities, we can mitigate the risks associated with fungal diseases and ensure better health for all.
Conclusion and Call to Action
In light of the critical issues surrounding antifungal resistance in fungal diseases, it is imperative to recognize the urgency of the matter. Throughout this article, we have examined the rising prevalence of antifungal resistance, the contributing factors, and the potential consequences of inaction. The data provided by leading scientists highlights a concerning trend that endangers public health across the globe. Early detection and intervention are crucial for managing fungal infections effectively and minimizing the development of resistance. Furthermore, the collaboration between healthcare providers, researchers, and policymakers is essential in formulating strategies to combat this growing threat.
One of the significant challenges in addressing antifungal resistance is the lack of awareness among the populace and even among some healthcare professionals. Increased education and dissemination of information are necessary to empower individuals to understand the importance of proper antifungal use and the dangers of misuse. Additionally, significant investment in research focused on antifungal therapies and resistance mechanisms will facilitate the development of new treatment options and management practices.
As advocates for health and well-being, we encourage readers to engage with this pressing issue. Consider sharing your thoughts, experiences, or questions regarding antifungal resistance in the comments section. Your input can contribute to a broader conversation and foster a greater understanding of this subject. Moreover, we urge you to advocate for increased attention from legislators and health organizations. By raising awareness and demanding action, we can collectively work towards a future where antifungal treatments remain effective and accessible, preserving public health for all.